7th January 2021
Models of Therapy: Comparing / Contrasting
As our understanding of the mental processes that occur during addiction has evolved, so have our therapeutic approaches in treating this “dis-ease.” Cognitive Behavioral Therapy has become increasingly popular for dealing with addiction, to the point where it now rivals the 12-Step approach as the “go-to” treatment for many clinics and practitioners. But there are numerous other approaches out there, each with their own set of adherents and detractors. Let’s take a look at the models sparking debate in today’s recovery landscape.
12 Steps And Cognitive Behavioral Therapy (CBT)
Since these are the two most well-known and frequently used therapeutic models in addiction therapy, we’ll begin by taking a look at how these approaches differ from each other, and whether they can be used in tandem.
One of the primary differences between the approaches is the “locus of control.” 12-Step models begin by pushing the addict to admit that they are “powerless” in the face of their addiction, while CBT is a method of self-help that aims to teach clients that they have the ability to regulate and control their own behaviors. The two attitudes are seemingly at odds, but as therapists at the Beck Institute note: “Patients sometimes ask us, “How can I take part in Cognitive Behavioral Therapy self-help if I have to admit to being powerless?” Our answer is that the “powerlessness” which they are acknowledging has to do with their prior behavioral and cognitive habits that were maintaining their problems with substances.” So while there is a philosophical difference between the two approaches, they can be reconciled.
Another seemingly large difference between the two methods is their guiding philosophies. The 12 Step program was initially inspired by the Oxford Group, a Christian organization which both Bill W. and Dr. Bob (the program’s founders) belonged to. As a result, spirituality is an essential component of the method, figuring prominently in the 12 Steps, 12 traditions, and Big Book. While strong efforts have been made to become inclusive of members of all faiths, agnostics, and even atheists, the spiritual component remains foundational to the movement. The 12 Step model is also based on the idea that addiction is a life-long condition without a cure, and that an addict will be an addict (hopefully in recovery) forever.
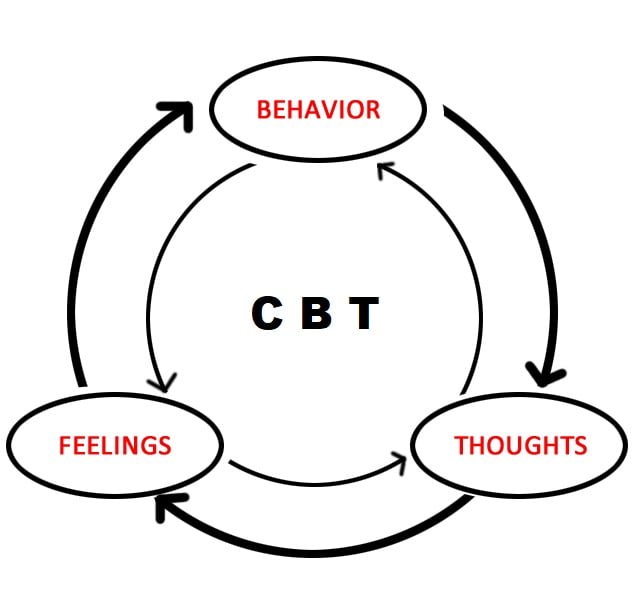
Meanwhile, CBT is based upon scientific principles rather than spiritual ones. It is meant to provide time-sensitive, practical solutions to a patient’s problems, whether with addiction, or any other disorder. It borrows components from a broad range of other therapeutic models but is essentially focused on identifying goals, and working towards them by recognizing and changing harmful patterns of thought and behavior. Simply put, the goal is to develop skills in recognizing what type of situation you’re in, moderating your thoughts and behaviors accordingly, and reacting in the way you desire. CBT models for treatment view addiction as an undesirable behavior that, when eliminated, is cured.
One final difference is the way each approach views harm reduction. The 12 Step model is based on absolute, life-long abstinence. Any slip in sobriety, even a single beer or joint, is viewed as a failure that puts the addict back to square one in treatment. CBT-based models, on the other hand, view their goal as allowing clients to lead healthier lives, and view any decrease in drug use or even a move to safer habits when using, as worthwhile goals and improvements which should be praised, and built upon.
While the differences in philosophy and approach are certainly significant, the two programs are certainly not irreconcilable. As one of our favorite precepts from the world of recovery states: “take what you need and leave the rest.” We’d guess that the majority of those in recovery have used elements of 12 Step programs and CBT in their journey to sobriety, and we’d recommend that you experiment with both and see what works for you.
SMART Recovery and The 12 Steps

Now that we’ve taken a look at the philosophical elements of both programs, let’s take a look at the differences in practice. The principles of CBT have inspired the SMART Recovery program, which can be either an alternative or a complement to 12-Step Programs. 12-Step meetings are led by peers and based on the principle of “sharing”, with participants offering their advice, experience, and struggles. In a 12-Step meeting, there is no “cross-talk”, meaning that you can’t comment on or criticize what someone else has shared. SMART Recovery meetings, on the other hand, are led by professional therapists or counselors, and cross-talk is allowed and encouraged. One powerful tool that the 12-Step model offers is the sponsor, someone who has been in recovery for a while and completed the steps, who provides advice, support, and fellowship with a newcomer. The sponsor is an extremely valuable resource for emotional support and they have proved crucially important for many recovering addicts and alcoholics.
The two approaches also differ in their conception of the addict’s journey to sobriety. In most 12-Step programs, individuals are encouraged to regularly go through the steps again. The idea that anyone in recovery is always in danger of relapse is common, hence the precept “too many years and not enough days,” which roughly means that an alcoholic or addict has become complacent, stopped actively practicing the steps, and relapsed. SMART Recovery, on the other hand, feels that those in recovery can become cured. As they write:
For many sincere participants there will come a time when attending our groups, or participating in our other services, is more in conflict with the pursuit of their life goals than enhancing them. Although these participants will always be welcome back if they want to come, this conflict signals that the time for graduation has arrived.
Other Alternatives
Existential Therapy

This form of therapy is based on the principles of existential philosophy as developed by thinkers such as Jean-Paul Sartre and Albert Camus. Treatment focuses on identifying questions relating to the meaning of life, the responsibilities, and freedom individuals have to make choices, and the individual’s place in the universe and society. This method of treatment is probably more valuable to individuals who are already on their way in recovery and are looking to find meaning in their lives and make positive choices.
Gestalt Therapy
Gestalt Therapy is based on the goal of pushing the patient towards an understanding of the present based on their current reality, rather than preconceptions based on what has happened in the past. The goal is to eliminate negative thought patterns and build awareness of the control and responsibility individuals have over situations and emotions. Gestalt Therapy employs guided visualizations to promote self-awareness and personal ownership while emphasizing that recollections of the past are inherently unreliable. The guiding philosophy is that self-awareness in the present will result in more positive choices relating to physical and mental health. Gestalt Therapy is a good option for those looking to move on from past traumas.
Holistic Therapy

Holistic Therapy is a broad umbrella that contains a wide range of treatments that are generally personalized for the patient. These treatments are most effective as a complement to other forms of therapy, working to rebuild the overall well-being of those in recovery and also deal with the symptoms of withdrawal. Yoga, Tai Chi, mindfulness practice, art therapy, equine therapy, exercise, nutrition, breathwork, and music are all examples of holistic therapy. While the benefits of holistic therapy may seem peripheral to treating addiction, rebuilding overall health, learning to practice self-care, and creating positive patterns of behavior are all extremely important elements of learning to live a healthy and sober life.
Naikan Therapy

Naikan is the Japanese term for “looking inside” or “seeing oneself through the mind’s eye.” The therapy was pioneered by Ishin Yoshimoto, a devout Buddhist who sought to offer a more accessible opportunity for everyone to benefit from the arduous self-reflection demanded by many Buddhist sects.
Naikan is designed to allow us to investigate and gain perspective on our relationships with ourselves, the other people in our lives, and the nature of existence. It is focused on three fundamental questions that define interpersonal relationships:
What have I received from ______?
What have I given to ______?
What troubles and difficulties have I caused ______?
Naikan has proved useful for those dealing with addiction because it allows the patient to let go of resentments, a source of emotional pain that is particularly damaging for those dealing with addiction. Many of those who practice Naikan come to realize how much others have contributed to their lives and cultivate an invaluable sense of gratitude towards those around them.
Person-Centered Therapy
Person-centered therapy is a form of treatment where the client takes the lead, and the therapist acts as a “compassionate facilitator.” In this form of therapy, the therapist refrains from steering conversations and judging or interpreting what is said. They’re meant to exhibit empathy and encouragement while encouraging you to listen to yourself and take control of your own life. Their role is to simply guide you through the process of self-exploration, allowing you to draw your own conclusions and grow on your own. This form of therapy is recommended for highly motivated people, as well as people who struggle with trust and self-confidence issues.
Therapeutic Communities

Therapeutic communities are generally long-term residences (though outpatient options do exist) that aim to use fellowship and peer-support to combat addiction. There are many different forms of TCs, some catering to individuals with dual diagnosis, the LGBTQ+ community, adolescents, and various other issues and populations. TCs leverage the power of many, and as clients progress through them they often are given positions of responsibility and even employment. The approach taken at these facilities is often described as “community as method”, where active participation in a household, and the responsibilities of social life “drive individual change and the attainment of therapeutic goals.” Therapeutic communities are especially beneficial to young people, those with severe addiction problems, and at-risk groups. They have also proven effective at boosting participation in aftercare. However, the structured, regimented nature of life in TCs and the time commitment involved mean that they aren’t the right solution for everyone.
Trauma-Informed Therapy
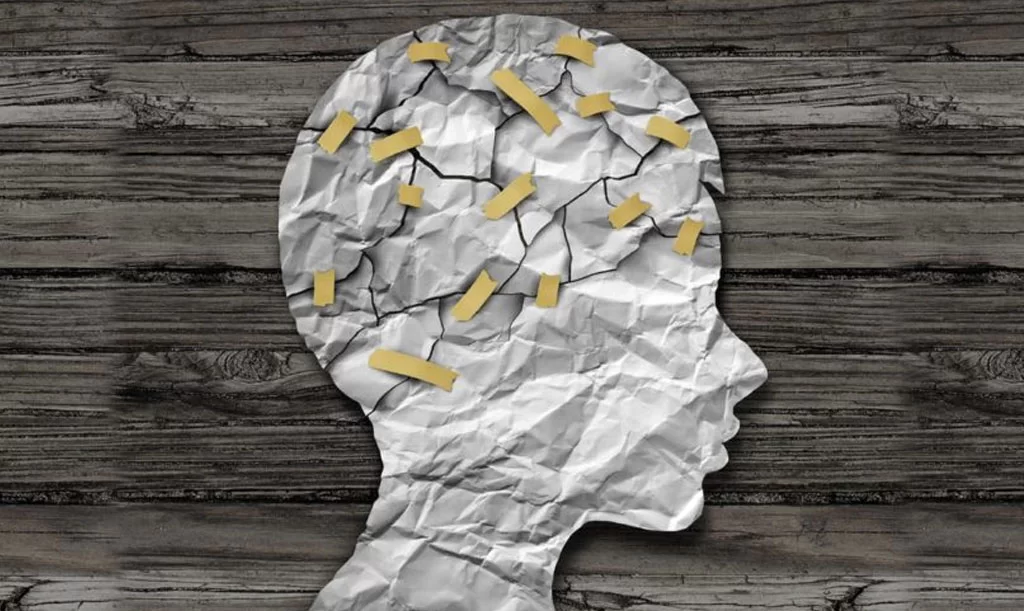
Trauma-informed therapy is a method developed by Dr. Stephanie Covington, among others, as a way to offer more effective treatment for health issues, particularly for women and girls. The American Department of Health and Human Services estimates that up to 99% of women in substance abuse treatment have suffered trauma, and both males and females who have suffered Adverse Childhood Experiences are far, far more likely to develop substance abuse issues. Trauma-informed therapy essentially entails that your treatment provider will have an awareness of how trauma reshapes the brain and alters responses to stressors, and uses that knowledge not to address the trauma, but its symptoms. Utilizing the strategies and techniques of trauma-informed therapy can be a game-changer in treating addiction, as it works to establish safety (defined as stability, adequate supports, and coping skills) before addressing serious issues and processing the roots of trauma. This approach minimizes the harms that can be caused by diving into painful memories and emotions before the patient has the coping skills to deal with them.
Next Steps

As you can see, there are myriad options for dealing with the pain which has driven your addiction, and the pain which your addiction has caused. We strongly recommend looking at all of them, and honestly assessing your personality and your needs before deciding on a course of treatment. Remember, there’s no harm in experimenting with different forms of therapy. If you have any questions about Naikan, kundalini yoga, or any of the other holistic options offered at Tabula Rasa Retreat, don’t hesitate to get in touch!
11th December 2020 • Sticky Post
Treatment for Dual Diagnosis: What You Need To Know
Dual diagnosis generally refers to an addiction that is complicated and exacerbated by a mental health disorder, and is often referred to as a “co-occurring disorder”. Both addiction and mental health disorders are notoriously difficult to treat. Both afflictions are rooted deep in neurological processes, past trauma, and genetic predispositions. When they combine they can have horrendous health consequences for sufferers. Medical studies have demonstrated that co-occurring disorders exacerbate and intensify the already brutal effects of addiction. Research shows that dual diagnosis individuals face challenges such as “greater exacerbation of psychiatric symptoms, medication nonadherence, an increase in aggressive and violent behaviors, poor personal hygiene, emergency room visits, and inpatient psychiatric placements.”
Properly identifying and creating diagnostic tools for identifying those at risk of or suffering from dual diagnosis is difficult. The symptoms of different mental illnesses are extremely varied, ranging from eating disorders to schizophrenia. And the stimuli provided by different substances can create a broad range of behaviors, symptoms, and actions. The National Alliance on Mental Health provides a list of signs that someone may be dealing with addiction and mental health issues, including withdrawing and isolating oneself from friends and family, confused thinking, sudden mood swings, loss of control over substance use, and engaging in risky behavior.
The most common psychiatric disorders associated with addiction and dual diagnosis are generally identified as
- Anxiety
- Depression
- Eating disorders
- Bi-polar
- Obsessive-compulsive disorder
- Schizophrenia
Many sufferers use substances to relieve the symptoms of their psychiatric ailments, and while this may seem to help in the short term, self-medication generally leads to substance abuse, a condition that leads to increased levels of anxiety and intensifies the symptoms of depression. As symptoms of mental health conditions worsen, individuals often become more reliant on drugs and alcohol, creating a negative cycle of dependence and despair.
Therapeutic Complications

One of the unique challenges in dealing with dual diagnosis is recognizing where problems are coming from. For instance, is the client depressed as a result of withdrawal, remorse over their actions, or an underlying mental issue? Dual diagnosis puts health-care providers in the position of trying to solve the classic “which came first, the chicken or the egg” question. It takes a real commitment from both the patient and the treatment provider to discover the root causes which must be addressed to allow for healing from co-occurring disorders.
Another challenge is that individuals with dual diagnoses present higher risks when put in stressful treatment situations. Statistics show that in the United States, a whopping 90 percent of those who commit suicide are struggling with depression, a substance use disorder, or a combination of the two. Dual diagnosis patients are also more likely to have violent tendencies, and attempt to harm others during treatment. So treatment providers need to have clearly established policies and procedures for maintaining the safety of patients and staff members in order to successfully deal with this thorny problem.
When treating dual-diagnosis disorders, it’s important that those involved be aware that the process will likely be longer and more complicated than traditional substance abuse treatments. Successfully dealing with drug addiction is a difficult and complex process in which relapses are quite common. When you add mental illness into the mix, care and patience are essential elements for healing. Don’t expect a quick fix or a magic bullet. The road to wellness could take months or years to travel, and having realistic expectations and committing to the process is essential for success.
Overcoming Dual Diagnosis
When attempting to treat co-occurring disorders, finding the right treatment provider is incredibly important. Integrating treatment is a fundamentally important element for dealing with dual diagnosis, and because treating these ailments is such an arduous and complex process, finding a facility that is experienced in dealing with these issues is highly recommended. Studies have shown that finding a treatment provider with the capability to treat both of your disorders under one roof can provide have a positive effect on treatment outcomes, and research has also shown that creating an individualized plan for dealing with dual diagnosis is a cornerstone of the most successful programs.
Cognitive Behavioral Therapy has also shown great promise for treating co-occurring disorders. The treatment, which focuses on teaching patients to unlearn hard-wired behaviors and change their self-perception and decision-making patterns, has changed the lives of thousands suffering from both addiction and mental health issues. Other alternative forms of therapy have also proven beneficial for dealing with the stresses and anxieties related to treatment and withdrawal. Yoga, mindfulness practice, and breathwork have all shown the potential to allow greater control of thoughts, “fight-or-flight” responses, and depressive tendencies.
Another treatment that has the potential to deliver massive benefits in treating dual diagnosis is iboga therapy. Many of the detrimental changes to brain chemistry and neural pathways that are caused by addiction and mental disorders can be re-set through iboga treatment. The substance has been shown to increase neuroplasticity, restore dopamine receptors in the brain to natural levels, and help individuals break free from toxic patterns of thought and behavior. The iboga experience can also offer relief from the symptoms of withdrawal, particularly for those addicted to opiates and opioids. This can allow patients to devote more of their energy to dealing with underlying mental health issues instead of focusing exclusively on breaking free from physical addiction.
Now What?

Everyone who suffers from a co-occurring disorder will have unique symptoms and hurdles to overcome in treatment. There are no easy solutions, but examining your own needs and challenges and finding an addiction treatment provider who can provide you with the resources that you need will greatly improve your odds of breaking free from this affliction. If you have any questions about our strategies for healing those suffering from co-occurring disorders, get in touch today!
6th November 2020 • Sticky Post
Understanding Psilocybin Therapy
The use of psychedelics in treating all manner of mental illnesses has been a hot topic in recent years. Scientists at prestigious institutions such as Johns Hopkins, New York University, the University of New Mexico, and Imperial College in London have conducted small but rigorous and controlled studies which have shown the immense potential of psilocybin therapy in dealing with depression, anxiety, and addiction. These studies have led to numerous books exploring the history and medical potential of psychedelics to change and heal the mind, most notably best-selling American author Michael Pollan’s “How To Change Your Mind.”
As momentum has built, a number of jurisdictions have decriminalized the cultivation and possession of psilocybin (the active ingredient in “magic mushrooms”), notably the major American cities of Oakland, California, and Denver, Colorado. 2020 will also see voters in Oregon and California decide on whether to legalize the substance throughout their states. Many psychologists, physicians, and people afflicted with mental illnesses are eager to take advantage of the benefits offered by this remarkable plant. As Mr. Pollan puts it:
a single psilocybin trip guided by trained professionals has the potential to relieve “existential distress” in cancer patients; break addictions to cigarettes, alcohol, and cocaine; and bring relief to people struggling with depression. Psychiatry’s current drugs for treating these disorders are limited in their effectiveness, often addictive, address only symptoms, and can come with serious side effects. Thus, the prospect of psychedelic medicine is raising hopes of a badly needed revolution in mental health care.
Psilocybin Treatment: The Process

Understanding Psilocybin Treatment
While there isn’t currently an established model for psilocybin treatment, most of the studies conducted thus far have patients use the substance in a controlled environment, supervised by a psychologist who guides them through the experience. The Imperial College study on depression offered patients a 25-milligram capsule of psilocybin, which is a substantial dose. They were placed in a room with a bed, surrounded with flowers and candles, and guided through traumas, significant past events, and formative memories.
A study at the University of New Mexico on psilocybin therapy for alcohol addiction offered participants four weeks of traditional psychotherapy, before giving them a dose of psilocybin in a quiet, comfortable room with male and female “co-therapists.” In this study, the therapists did little more than direct patients to “turn their attention inward” and go where their minds took them. This was followed by four more weeks of psychotherapy, another psilocybin session, and a final bout of traditional therapy.
As one participant noted, his experience wasn’t focused on his dependence on alcohol, but rather on the stresses, guilt, and happiness which his relationship with family members created. His recovery wasn’t motivated by a desire to avoid alcohol, but rather by the prospect of improving his relationships with loved ones. He reported being effortlessly abstinent for months afterward, before beginning to drink moderately once again but with “a conscientiousness he had never experienced with alcohol before.” Two years after the study his drinking remained under control, and he had repaired his marriage and relationships with his children.
Why is Psilocybin Treatment Effective?
Why is Psilocybin Treatment Effective?
While many countries are accelerating research into psilocybin therapy, no one is exactly sure why the treatment has proven to be so effective. Nonetheless, there are a number of compelling theories as to why it works. Serotonin is often cited as one possible key to the effects of psilocybin, as the substance causes “downregulation” of the serotonin system, which can result in reduced impulsivity and improved mood. But changes to serotonin typically last for just one week, so the longer-term benefits of the treatment must derive from a different source.
Michael Bogenschutz, the lead investigator in the University of New Mexico alcohol trial, posits the view that exposure to psychedelics and oneirogenics can create a phenomenon that mirrors the long-tail effects of PTSD. As he puts it:
"there's a whole process that happens when a toxic memory is seared into the brain. The only physical effect is probably light hitting the eyes. It's the meaning made of that memory, and the brain and body's reaction to the meaning, that can cause lasting damage. So if there are experiences that are so toxic and so horrible that they can cause physical and psychological damage, it's not a crazy idea that there are some experiences that are so positive, so beneficial that they can have a healing effect."
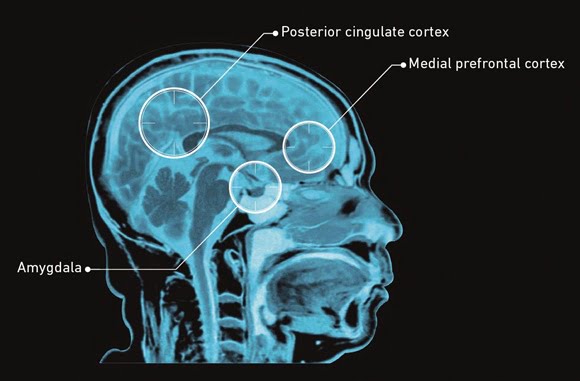
Other researchers point to the concept of “ego death” that has long been associated with psychedelics. Robin Carhartt-Harris, a researcher at Imperial College, notes that psilocybin reduces activity in the brain’s “default mode network”, a collection of brain regions and neurotransmitters that are believed to construct an independent self and place it at the center of perceptions and experiences. Psychedelics help individuals to pay less attention to the self, breaking down walls and facilitating connections. Since many depressed and addicted people are plagued with a deep and abiding sense of isolation from others, this can feel like a dramatic escape from a mental prison. Many of the participants in these studies reported that psilocybin dramatically reduced their sense of alienation.
Another theory is that the therapy increases neuroplasticity, changing and reshaping neurons in the brain. This remodeling of cells is the basis of all learning, and substances like psilocybin and iboga have been proven to improve neuroplasticity. Addiction, anxiety, trauma, and depression can create negative changes in brain chemistry, as the mind learns to take pleasure or stress from external cues. Psilocybin seems to help restore the brain to a pre-addicted state.
Psilocybin Treatment: Safety Concerns

Psilocybin Treatment: Safety Concerns
While psilocybin therapy has shown immense promise to heal mental wounds, we would strongly recommend restricting its use to a clinical setting. There are physical and psychological risks that go hand in hand with the benefits of psychedelic therapies, and in many jurisdictions, you can be arrested and incarcerated for use or possession of these substances. Michael Pollan notes that in all societies that used psychedelic substances, ranging from the Amazon to ancient Greece, they were always used with “deliberateness and care.” He writes that these substances “were not taken alone but usually in a group under the direction of an elder or shaman familiar with the mental territory, and they were used only on certain occasions, surrounded by ritual and with a clear intention. There was nothing casual about it.” All would be wise to maintain this level of caution as they experiment with their immense potential.
To find out more about what psilocybin therapy can do for you, contact us now!
