16th December 2020 • Sticky Post
Detox: 12 Alternative Options To Consider
If you were in need of heart surgery, you probably wouldn’t be satisfied with choosing a method devised between 1939 (the year AA’s Big Book was published) and 1953 (the year in which NA was founded). But in the field of drug detox, many providers, patients, and professionals are content to adhere to the established model of cold turkey, talk therapy, and regular attendance at 12 Step meetings. While this model has worked for thousands upon thousands of sufferers, it has also allowed many people to fall through the cracks, their needs unmet and their challenges too great to be adequately addressed by these detox/treatment modalities.
New strategies and techniques for detoxing off of drugs are sprouting up every day, but many in the treatment field are still relying heavily on either cold-turkey or methadone and other long-term opioid replacement drugs which can create as many problems as they solve. At Iboga Tree Healing House, we feel that it’s worthwhile to take a long look at all of the other strategies, methods, resources, and treatments available for those looking to detox from their addiction. There are a lot of alternatives out there, and some of them are worth exploring, particularly if other treatments haven’t worked.
1) Ayahuasca Detox

Ayahuasca is a powerful psychoactive substance that has been used for religious and medicinal purposes in the Amazon basin for millennia. Addiction expert Dr. Gabor Mate has sparked debate by using the substance to treat addiction. Advocates claim that it can help people to explore and heal from the traumas and stresses that have fed their addictions while prompting meaningful connections with others, as well as spiritual growth. As with most psychedelic and oneirogenic treatments, ayahuasca treatment doesn’t just involve using the substance, but it is generally accompanied by pre-and post-treatment therapy sessions, as well as being guided through the use of the substance by an experienced practitioner. Ayahuasca’s effects include changes to the amygdala and insula that have been reported to reduce depression and anxiety, and it also helps to normalize levels of serotonin, a chemical that regulates mood and effects pleasure-seeking urges which are related to substance use. The substance appears to be particularly helpful in treating alcohol and cocaine dependence.
2) Cannabis-Assisted Detox

Recent medical studies have found that cannabis is capable of reducing the effects of opioid withdrawal. While the evidence is still described as “nascent” by researchers, numerous studies have shown that cannabis and cannabinoids decrease the symptoms of acute opiate withdrawal. In some studies, those going through withdrawal reported that cannabis had alleviated withdrawal symptoms when opioid replacement therapy was not sufficient. But other studies have produced conflicting evidence, and the process through which cannabis aids in withdrawal is reportedly “murky and complex.” Meanwhile, studies conducted on rats have found that CBD “has been shown to reduce the rewarding aspects of multiple drugs of abuse, such as cocaine, amphetamines, and nicotine.” While cannabis and cannabinoids show potential, it’s too early to determine how much they can aid in withdrawal.
3) Abstinence / Harm Reduction
Abstinence-based models for treating addiction are based on the total avoidance of all mood and mind-altering substances. Abstinence based models are focused on creating a lifetime of sobriety and generally base themselves on the 12 Steps. They define addiction as a chronic and incurable condition that can become dormant but will require treatment and maintenance over a lifetime. Abstinence-based models would dismiss pharmacological and psychoactive substances that aid in lessening the symptoms of withdrawal.
Harm reduction, on the other hand, is focused on minimizing the effects of drug use rather than emphasizing the importance of sobriety. Harm reduction principles are based on the idea that abstinence might not be the best answer for all individuals and communities, and that services and resources for addiction should not be judgemental or coercive. Advocates of harm reduction feel that condemning drug use and drug users are counterproductive strategies, and that drug use is a fact of life that is intimately connected to socio-economic realities. They would recommend treatment strategies that employ psychoactive substances which can aid with withdrawal and treatment.
4) Heantos-4 Detox
Heantos-4 is a compound of herbs that is currently used to treat opioid addiction in Vietnam. It is reported to have beneficial effects on withdrawal and relapse prevention, as well as providing sedative effects during detox. Studies on animals have shown that the compound has neurological and physiological effects that correlate with the anecdotal evidence of its benefits to the addicted. Advocates claim that the substance boosts the production of GDNF hormones in the brain, creating enhanced neuroplasticity that can offer a wide range of benefits to the addicted. Meanwhile, there are reports that this compound has caused numerous deaths in treatment at Vietnamese clinics.
5) Iboga Detox

Iboga is the root bark of the tabernanthe iboga plant native to west and central Africa. It has been used for centuries in the region’s Bwiti spiritual tradition for medicinal and ritualistic purposes. Decades ago, American heroin addict Howard Lotsof used the substance to break free from heroin addiction and has spent the years since advocating for its use as a medicine. Iboga has been proven to dramatically reduce withdrawal symptoms from opiates and opioids, as well as reducing cravings for a time ranging from 3 months to one year following its use. It has also been shown to increase the brain’s production of the GDNF hormone and reset dopamine receptors to a pre-addicted state. In large doses it has caused seizures, and it can exacerbate pre-existing heart conditions, but it still appears to be safer to use than methadone.
6) Kambo
Kambo use is associated with traditional rituals from the Amazon region which use a poison (Kambo) secreted by giant monkey frogs in order to facilitate a number of health benefits. Proponents claim that benefits include increased stamina, heightened senses, and cleansing properties. Kambo contains small proteins called tachykinins which affect “reward, motivation, and stress responses in the brain.” These proteins can bind to receptors in the brain, which can, theoretically, have a profound effect on addiction. However, Kambo skeptics would point out that the substance is a poison which can have serious, and even fatal, side effects, and that a lack of clinical evidence on its workings makes its use unsafe at this juncture.
7) Ketamine-Assisted Detox
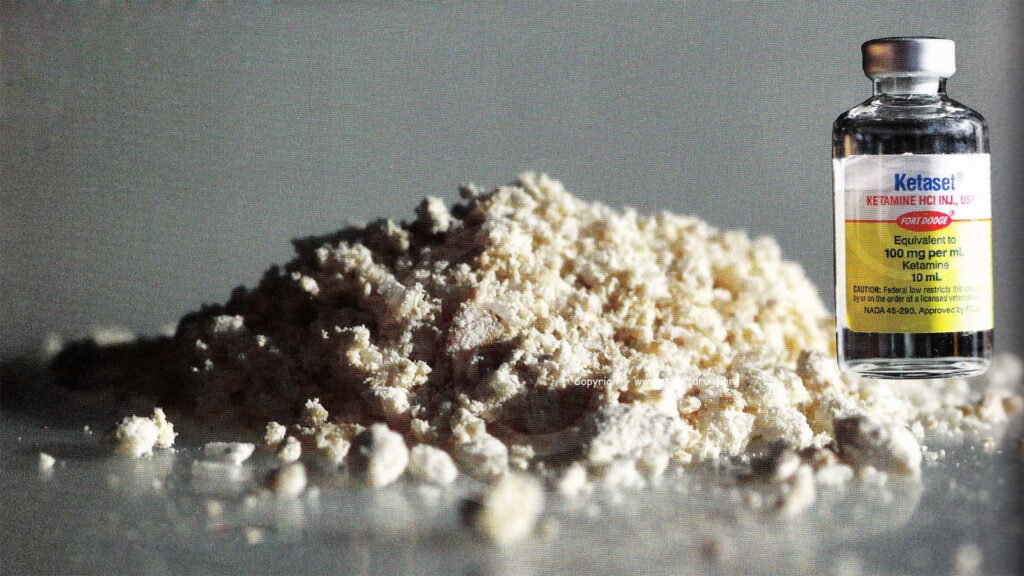
Most people think of ketamine as a drug of abuse, but it is also a potent painkiller that is regularly used by anesthetists and pain specialists. There is evidence of ketamine being used to treat patients who had developed a dependence on opioid-based painkillers such as oxycontin. In many cases, ketamine use minimized the effects of opioid withdrawal, and then patients were weaned off of ketamine with minimal withdrawal symptoms. While ketamine use has the potential to create a new addiction, it could be the lesser of two evils for patients who’ve developed opioid dependence.
8) Kratom- Assisted Detox
Kratom is a tropical plant grown in Southeast Asia which has long been used as a painkiller and mild stimulant. It is also an opioid agonist, meaning that it stimulates the same receptors as opioids, and is now being used to lessen the symptoms of opioid withdrawal. Its effects have been praised by many recovering addicts, but it can create dependence if used heavily, and side-effects can include hallucinations, paranoia, hypothyroidism, and liver damage. Because kratom is currently sold as an herbal supplement in many countries, it is easily accessible, but should be used with caution. The evidence for kratom’s effectiveness is currently just anecdotal, since clinical studies have yet to be completed.
9) NAD+ Therapy
NAD+ is a naturally occurring co-enzyme of niacin which has demonstrated promise as a treatment for substance abuse disorders. Studies have shown that addicts generally have very low levels of NAD+ in their systems, and many of the physical and mental disorders that frequently co-occur with addiction have been proven to deplete the body’s store of this essential nutrient. Proponents of the treatment tout its ability to restore the balance of neurotransmitters, which is disrupted by the process of withdrawal, decreasing withdrawal symptoms and cravings
NAD+ works in theory because it creates “neuroplasticity”, the brain’s ability to create new neural pathways and heal itself. Years of addiction condition the brain to release dopamine when given substances of abuse, and to respond to stress, pain, and anxiety by treating them with drugs and alcohol. NAD+ can help to change the structure of the brain, offering addicts the chance to gain pleasure from activities other than substance abuse and to find new ways to cope with the stresses of life.
10) Psilocybin-Assisted Detox

As with many of the substances on this list, psilocybin therapy is associated with increased neuroplasticity and beneficial changes in brain chemistry. Various studies have found that psilocybin therapy helps those suffering from depression and alcohol dependence, though the exact mechanisms by which it works aren’t yet known. As a participant in one study on psilocybin’s effects on alcohol abuse noted, his experience wasn’t focused on his dependence on alcohol, but rather on the stresses, guilt, and happiness which his relationship with family members created. His recovery wasn’t motivated by a desire to avoid alcohol, but rather by the prospect of improving his relationships with loved ones. He reported being effortlessly abstinent for months afterward, before beginning to drink moderately once again but with “a conscientiousness he had never experienced with alcohol before.” Two years after the study his drinking remained under control. The changes to the ego, a renewed sense of connection with others and with one’s true self, and changes in brain chemistry are all touted by advocates of psilocybin therapy, and the news is reaching the mainstream, as this recent “60 Minutes” report shows.
11) Rational recovery
Rational Recovery is a program created by California social worker Jack Trimpey which is designed as an alternative to 12 Step programs. It appears to be based somewhat on CBT, as it identifies what is referred to as the “Addictive Voice” as the driver of substance abuse. The Addictive Voice is essentially a thought process that steers the addict towards the object of addiction without regard for consequences, health, or responsibilities. Rational Recovery aims to teach the addict to recognize and ignore thoughts and impulses created by the addictive voice, and to create patterns of thought and behavior that enable a healthy life. Rational Recovery did not include religious or spiritual principles and regarded addiction as a voluntary behavior rather than a disease. Although the movement officially ended in the early 2000s, many of the ideas espoused were adopted by SMART Recovery.
12) 12-Step and SMART Recovery Programs
We’ve written before about the contrasts between these two models for peer support organizations, and both have a lot to offer addicts in recovery. Philosophically, one of the major differences is that SMART Recovery is built on a foundation of scientific principles, while 12 Step Programs favor spirituality. Because of this, 12 Step groups encourage their members to admit that they’re powerless in the face of addiction and call on a higher power, while SMART Recovery uses the principles of Cognitive Behavioral Therapy to encourage individuals to take control of their own thoughts, behaviors, and actions to build a positive life.
Proponents of the 12 Step model also believe that the principles they follow are universally applicable to all addicts, while SMART Recovery allows members to create their own approach based on age, gender, emotional needs, and other considerations. 12 Step meetings are generally facilitated by peers who have no special status or authority, while SMART Recovery meetings are led by professional therapists. The principles of SMART Recovery also allow for the idea of being “recovered’, while 12 Step adherents feel that addiction is an incurable disease that the addict must live with and manage for their entire life. In our view, the greatest advantage of 12 Step groups is the presence of a sponsor, a peer experienced with life in recovery who commits to offering you guidance and personal support. SMART Recovery, on the other hand, benefits from being committed to evolving with the latest advances in pharmacology and neuroscience, adapting its approach to treatment as we learn more about the nature of addiction.
Investigate!
As you can see, you have a plethora of options to choose from if you feel you need a push down the road to recovery. While we at Tabula Rasa Retreat wouldn’t recommend every new approach that’s out there, we do advise all addicts to find an approach that matches their unique needs. It won’t be easy, but with the right approach, you can beat your addiction. If you’d like to discuss any method for living a healthy, sober life with us, we’d be happy to open a dialogue with you!
3rd November 2020 • Sticky Post
Opioid Replacement Therapy: Weighing the Costs/Benefits
Opioid Replacement Therapy (ORT) is a way to lessen the impact of addiction to opiates and opioids by replacing dangerous drugs like fentanyl and heroin with legal, long-acting, non-euphoric drugs such as methadone and suboxone. Advocates cite a host of benefits that can be obtained through Opioid Replacement Therapy, including reducing the risk of HIV transmission, overdoses, and crime, while helping the addicted to hold down jobs and maintain functional relationships. Opioid Replacement Therapy also theoretically keeps individuals in treatment by reducing the symptoms of withdrawal and the cravings for illicit drugs. It sounds appealing, and methadone has been a popular treatment for years. The World Health Organization has labeled it an essential medicine, and it’s used without question by health-care providers the world over (almost 50,000 kgs. of it are manufactured every year). But is ORT really the best way to treat opioid addiction?
Methadone: Pros and Cons

Opioid replacement therapy: weighing the pros and cons
As a long-acting opioid, as well as an opioid agonist, methadone ensures that the user typically needs a single daily or bi-daily dose and that they cannot experience highs even if they use other opioid drugs. This allows those who use the substance to return their lives to some sort of normality. Since most users are obtaining a single dose every 24-48 hours in an outpatient setting, they are free to go about their daily business unencumbered from intoxication or the need to secure more drugs. Furthermore, enrollment in an opioid replacement program generally nudges the user towards meaningful interactions with the health-care system which can successfully steer them towards a more complete recovery.
A study from Harvard University’s medical school found that approximately 25% of methadone users would successfully wean themselves from the substance over the long-term, 25% would continue using it indefinitely, and 50% would eventually return to their previous addiction. A 2009 study from the Cochrane Review concluded that methadone treatment increases the chance of successful treatment outcomes by helping to retain patients in treatment and that it decreases heroin use compared to programs that don’t offer opioid replacement therapy. The study also found that methadone didn’t actually decrease the risk of mortality or prevent criminality in a statistically significant way.
While methadone programs offer some substantial benefits to those grappling with addiction, they come with substantial side-effects and risks. Common side-effects include nausea, vomiting, sexual dysfunction, slowed breathing, and itchy skin, and there is some evidence that prolonged use can cause a number of lung and respiratory issues. Meanwhile, neuroscientists are still discovering the effects methadone use has on the brain, as experiments with rats have shown that a three-week course of methadone led to a “significant” – 70 percent – reduction of a signal molecule that supports memory and learning in the brain’s frontal lobe and hippocampus. Methadone is also a deeply addictive substance, which causes worse withdrawal symptoms than the heroin that it replaces. And the risk of overdose doesn’t go away for those using methadone. In fact, the American Center for Disease Control reports that methadone is to blame in a full third of all prescription painkiller related deaths occurring in the USA.
Methadone has helped many addicts by acting as a first step towards recovery, offering a measure of stability in their lives, and enticing them to interact with recovery professionals. But the side-effects and risks associated with its use are deeply concerning, and there are other options available for those looking for ORT.
Naltrexone and Buprenorphine

Naltrexone and Buprenorphine
Like methadone, buprenorphine is a synthetic opioid that can reduce or curtail the symptoms of withdrawal. Suboxone, the most common variety of buprenorphine, also contains a substance called naloxone, which causes serious and deeply unpleasant side-effects if the substance is injected. It is included to reduce the potential for abuse. Suboxone was approved for use by the American Food and Drug Administration in 2002, and it has become incredibly popular. In 2013 the drug made $1.55 billion in sales, more than Adderall and Viagra combined!
Buprenorphine treatment has some significant advantages over methadone. It has less potential for abuse because of the inclusion of naloxone. It has also proven to be a safer alternative. A 6-year study conducted by researchers in England and Wales found methadone was more than 6 times more likely to cause overdose deaths than buprenorphine, with 2,366 mortalities associated with methadone use, and only 52 related to buprenorphine.
Naltrexone is another synthetic opioid that was originally intended for use in pill form. The American government concluded that it “does not produce tolerance or withdrawal. Poor treatment adherence has primarily limited the real-world effectiveness of this formulation. As a result, there is insufficient evidence that oral naltrexone is an effective treatment for opioid use disorder.” However, in 2010 an extended-release, injectable form of naltrexone was approved by the FDA. This version requires a single injection per month and has been found to be as effective as buprenorphine in reducing opioid use. However, withdrawal from opioids must be completed before this type of naltrexone is safe to use, which is a significant barrier for many addicts.
Buprenorphine and naltrexone can offer a sufferer the benefits of methadone treatment, along with reduced risk of overdose, death, and abuse. However, like methadone, they are imperfect solutions that can help addicts to manage their affliction and lead them into treatment but also create a new dependence that can take years to break free of.
Effective Alternatives

Opioid Replacement therapy: weighing the costs and benefits
You may already know about Iboga’s ability to treat withdrawal symptoms and substance cravings, as well as its remarkable restorative effects on the brain. If you don’t, you may want to read this post on iboga’s effectiveness in treating opioid addiction. In addition to its clinical benefits, the substance induces an ego-free, reflective state that can also help addicts deal with past trauma and certain mental health issues.
Unlike methadone, iboga isn’t habit-forming and is extremely unlikely to be abused. There is no evidence that it is physiologically or psychologically addictive. While systematic, controlled clinical trials in the US and Europe have yet to be conducted (mainly because the substance is classified as a Schedule I drug), there are countless testimonials from people who credit iboga with saving their lives and allowing them to escape from addiction.
Iboga use is not without risk. It can exacerbate pre-existing cardiac conditions, and in abnormally large doses it may induce seizures. But even though it is often self-administered, or used in unsafe settings due to its murky legal status, it is still safer than methadone, causing 1 death in every 427 reported treatment episodes, compared to a 1:364 mortality rate for methadone.
5th December 2019
The Opioid Epidemic: Calculating the Costs
The opioid epidemic continues to impose a tremendous human and societal cost on the world. Big pharmaceutical companies have gotten us into a horrendous mess by dishonestly, unethically, and even illegally pushing opioid painkillers on a public that was unaware of the significant risks of dependency and addiction. Purdue Pharma, the maker of Oxycontin and an industry leader who reaped immense profits from peddling dangerous drugs, recently settled a lawsuit in Oklahoma for a whopping 270 million dollars. There are still approximately 2000 other lawsuits waiting to go to trial across the United States, alleging that Purdue and other large pharmaceutical companies “engaged in deceptive marketing that downplayed the addiction risk from opioids while overstating their benefits.” Before the financial settlements and jury awards start to roll in, let’s take a long look at the human and financial costs of the opioid crisis.
The Pain Paradox

The opioid epidemic has roots not just in irresponsible marketing campaigns, but in the structures of our health-care systems and societal approaches to dealing with pain. In America, HMOs have largely replaced family physicians, and doctor-patient interactions have shifted from intimate, familial relationships focused on long-term health to a customer service model. Meanwhile, funding for holistic, multi-disciplinary approaches to pain management has dried up in many countries. These trends created the conditions which allowed opioid use to spread like wildfire.
Rather than addressing the root causes of pain and working on long-term solutions, physicians (and dentists, the most common issuers of fast-acting opioids) settled on temporary pain relief via pills. Everyone involved with the health-care system was incentivized to settle for oxycontin instead of pursuing the more expensive, complicated, and slower psychosocial and physical solutions that would enable the afflicted to successfully manage their pain.
The Opioid Epidemic's Terrible Human Toll
According to the American Centers for Disease Control, over 700,000 people died of drug overdoses between 1999 and 2017, with 68% of the deaths (almost 400,000 fatalities) involving an opioids. By 2017 the number of deaths involving opioids was 6 times higher than it had been in 1999, and 130 Americans were being killed by opioid overdoses every day! Americans are now more likely to die from an opioid overdose than from a car crash.
Opioid prescriptions were frequently given not just for severe long-term pain, but also for routine procedures which caused a few days of manageable pain, like wisdom teeth removal, bone fractures, and minor surgery. Relying on pills to avoid a few days of discomfort led millions to years of addiction and even death. As evidence mounted that exposure to opioid painkillers heightened the risk of abuse and addiction, the prescriptions continued to pile up.
Nowhere was harder hit by the opioid epidemic than rural communities in America. The state of West Virginia alone was showered with 780 million oxycodone and hydrocodone pills, amounting to “433 pills for every man, woman and child” in the state. One town with a population of 392 and a single pharmacy received 9 million pills in a two year period. Kanawha County, with a population of 190,000 received 66 million oxycodone and hydrocodone pills.
Pharmaceutical companies and legislators were finally forced to address the issue and limit the supply of pills, but that has led to even worse problems. As the legal supply of opioids has dried up, more and more addicts have turned to the black market, which is largely comprised of Fentanyl-based pills. Fentanyl, a powerful synthetic opioid, is manufactured in China, shipped to Mexico where it is processed into counterfeit pills, and distributed around the world. Fentanyl is 30-50 times stronger than heroin and can be lethal in doses of just 2 milligrams. As a US Attorney in Ohio has noted: “One of the truly terrifying things is the pills are pressed and dyed to look like oxycodone. If you are using oxycodone and take fentanyl not knowing it is fentanyl, that is an overdose waiting to happen. Each of those pills is a potential overdose death.”
The Financial Cost of the Opioid Epidemic
A report from Altarum, an American healthcare research and consulting firm, calculated that eliminating opioid addiction and overdoses would create an annual benefit to the US economy of $115 billion. They calculate that the total cost of the opioid epidemic since 2001 has been over $1 trillion and that an additional $500 billion will be added to the sum by 2020. Others calculate the cost to the government alone at approximately $80 billion annually, without even factoring in the cost of healthcare fees, legal expenses, and lost productivity on individuals and families.
These immense sums boggle the mind, but they fail to reckon with the profound impact of the opioid crisis on communities. Trauma, fractured families, decreased property values, loss of community well-being, educational impacts, and a myriad of other social problems whose impact has yet to be gauged are on their way. The opioid crisis has left behind it a wake of devastation, poverty, and heartbreak. But is there anything that can be done to reverse the tide of human misery?
What's Next?

One necessary step for dealing with the current opioid crisis is embracing the principles of harm reduction. The medical establishment has led millions of people toward addiction by profitably over-prescribing pills. Their victims shouldn’t face criminalization and stigma for following a doctor’s advice. The Portuguese model has shown great promise for dealing with addiction by treating addiction as a health issue. It’s time for other countries to follow suit.
Another important tool for dealing with rampant opioid addiction is iboga therapy. The treatment is a proven success in dealing with substances such as Oxycontin and Oxycodone, acting as an addiction disruptor and opioid antagonist. If governments are serious about battling the plague of opioid addiction, the time to begin clinical trials is now!
But perhaps the most necessary step in dealing with this massive crisis is changing our understanding of pain. Pain management is a necessary part of life, and all of us will have to deal with intense physical and mental pain at some point. It’s time for the medical establishment to embrace comprehensive, holistic pain management plans. Pressure, stretching, motion, and touch are all proven to relieve pain. Cold and vibration-based therapies have been clinically proven to limit opioid use and dull perceptions of pain while the body heals. Sleep hygiene, ibuprofen, magnesium supplements and a host of other options have shown to be as or more effective than opioids in dealing with certain varieties of pain. As Dr. Amy Baxter of Pain Care Labs argues, changing the paradigm from a focus on pharmaceuticals to creating comprehensive, individual “pain plans” will destroy the false dichotomy of pills and “complementary” treatments. There isn’t a “Big Yoga Lobby” taking doctors on expensive promotional junkets yet but using some of the windfalls from lawsuits against pharmaceutical companies to create one wouldn’t be a bad idea.
29th August 2019
The State of the Opioid Crisis in 2019
The opioid crisis has continued to run unabated, despite the efforts of lawmakers, treatment providers, and healthcare professionals. Americans are now more likely to die from an overdose than a car crash. And as this recent article in US News and World Report states, the opioid epidemic has become America’s “deadly new normal” with no end in sight for the current, historically high rates of addiction, overdoses, and deaths. Let’s take a look at where we stand with the opioid crisis, and how we are moving forward.
Are new regulations having an impact?

Many analysts would trace the growth of the opioid crisis to Purdue Pharma’s aggressive marketing of OxyContin as a painkiller. The drug was made for patients suffering from moderate to severe pain, but a sales force that irresponsibly downplayed the substance’s potential for abuse led many health professionals to over-prescribe the drug. As detailed in this article in the American Journal of Public Health, Purdue Pharma’s sales force was armed with research that dramatically downplayed the risk of addiction, and convinced doctors and dentists that OxyContin was an effective, low-risk option for pain management.
US News and World Report notes that a decade after the introduction of OxyContin, regulators had yet to take the spread of opioid addiction seriously. A 2011 report from The Institute of Medicine on pain relief was longer than 350 pages, yet only mentioned addiction a few times. As FDA Commissioner Dr. Scott Gottlieb has stated: “The old notion was that if you were using opioids for a legitimate purpose, you couldn’t become addicted. We now know that’s not true.”
Meanwhile, pharmaceutical companies were making massive profits by flooding small towns with millions of addictive pills. This scathing report from an American Congressional Committee, which found that distributors and the DEA “failed to abate [the] US opioid crisis,” details how pharmaceutical giant McKesson shipped 9650 hydrocodone pills per day to a pharmacy in Kermit, West Virginia, a town with a population of just 400! These shipments were 36 times above the companies own monthly dosage threshold.
The American DEA is still attempting to work out a “centralized way to analyze suspicious order reports”, but earlier this year they approved a rule change that requires drug producers to identify a legitimate need for opioids to justify their rates of production. This new regulation is an attempt to limit the supply of pills, but it’s too early to judge its effectiveness
Meanwhile, pharmaceutical companies are facing lawsuits from various levels of government across America for failing to detect and report suspicious orders of pain pills. McKesson has already paid $150 million to settle a federal complaint about negligence, and they have agreed to a multi-year suspension from sales of controlled substances in four states. Sixteen states and hundreds of cities and counties are currently suing pharmaceutical companies for the negligence and aggressive, misleading marketing campaigns that brought the crisis to its current, deadly state. As Mississippi Attorney General Mike Moore states “Should taxpayers pay to clean up the mess caused by multi-billion dollar companies who lied to sell their products, or should the companies who profited pay?”
Mounting Tragedies
While it’s certainly a positive development that governments are taking legislative and legal action to fight the spread of addiction, it will be a while before these actions have their effect. In the meantime, those already afflicted are in increasingly dire straits. As the supply of legal pills dries up, more and more users will turn to counterfeit prescription opioids, pills that are often laced with, or made entirely from, fentanyl. The Partnership for Safe Medicines has found counterfeit pills containing fentanyl in 44 of the 50 US states, and deaths attributed to those pills have occurred in at least 26 states. In 2017 over 275 million packages flowed through the American government’s international mail facilities, and authorities estimate that 9% of them contained drugs of some kind. In a report on the situation, the FDA noted that currently only 10,000 packages are inspected each year.
Even if governments can dramatically reduce the legal supply of opioids, the opioid crisis could worsen. It’s estimated that over $800 million dollars worth of fentanyl has been shipped from China to the US in the past few years, and this is bad news for any opioid addict or anyone who cares about one. Fentanyl is 30-50 times stronger than heroin and can be lethal in doses of just 2 milligrams. As a US Attorney in Ohio has noted: “One of the truly terrifying things is the pills are pressed and dyed to look like oxycodone. If you are using oxycodone and take fentanyl not knowing it is fentanyl, that is an overdose waiting to happen. Each of those pills is a potential overdose death.”
Here's The Good News

It is a positive step forward that governments, the courts, and even pharmaceutical companies are finally taking action to contain the current opioid crisis. Furthermore, Chinese Leader Xi Jinping recently pledged to declare fentanyl a controlled substance and clamp down on its production and sale. But for those already facing the nightmare of opioid addiction, that is cold comfort. The only way to stay safe is to seek treatment and build a healthy, sober life without the painkillers that are causing 130 Americans to die every single day.
And on this front, there is good news. Exciting new treatments such as iboga, suboxone, and ayahuasca are helping many addicts with the withdrawals and cravings that make getting sober so difficult. Iboga has proven to be particularly effective in treating short-action opioid withdrawals, including commonly abused substances such as codeine and oxycodone. Because these drugs leave the system quickly, the treatment can be administered during the early stages of withdrawal, where it minimizes the horrific symptoms associated with quitting “cold turkey.” Ibogaine also resets dopamine receptors in the brain to a pre-addicted state, normalizing the addicts’ ability to experience pleasure and significantly lowering their tolerance for opioids.
Addictions thought leader Dr. Gabor Maté believes that “A hurt is at the centre of all addictive behaviours. It is present in the gambler, the Internet addict, the compulsive shopper and the workaholic. The wound may not be as deep and the ache not as excruciating, and it may even be entirely hidden—but it’s there.” Addictions experts across the globe are gaining an ever greater understanding of the roots of addiction, a dis-ease which often begins as a response to mental and physical pain. Millions turned to opioids in response to chronic physical and emotional pain. But the relief that they offered was temporary, and the horrifying toll they have taken on our societies has been huge. If you’re ready to end the nightmare of opioid addiction, don’t hesitate to get in touch!


